By Grace Liao
Asian Scientist
October 27, 2011
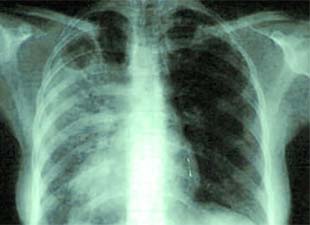
A clinical trial in Cambodia has shown that starting antiretroviral treatment for HIV at two weeks, instead of two months after tuberculosis treatment, increases survival rate by 33 percent in HIV-TB co-infected patients.
Asian Scientist (Oct. 27, 2011) – Timing is everything when treating patients with both HIV and tuberculosis, as demonstrated by researchers at Children’s Hospital Boston and the Immune Disease Institute (IDI) via a large-scale clinical trial in Cambodia.
The study results show that immunosuppressed HIV-TB co-infected patients should be started on ART rapidly at two weeks, rather than two months as current practice, after beginning TB therapy to increase survival rate by 33 percent.
These results were published in the October 20 issue of the New England Journal of Medicine by Prof. Anne Goldfeld of the IDI and Children’s Hospital Boston, and the CAMELIA (Cambodian Early versus Late Introduction of Antiretrovirals) study team.
A collaboration of Cambodian, French, and American physicians and researchers, the CAMELIA trial set out to settle a long-standing debate in the medical community over the relative timing of ART and anti-TB treatment regimens in co-infected patients.
Some have advocated for delaying ART for upwards of two months after initiating anti-TB treatment. They argue that the toxicity of and difficulties in adhering to the two regimens (which together require patients to take seven pills every day), as well as the risk of severe inflammation as the immune system rebounds from HIV’s suppressive influence, create undue burden on patients.
Conversely, those supporting early initiation of ART note that rapid restoration of immune function bolsters the effects of anti-TB treatment.
Latest World Health Organization (WHO) guidelines recommended that co-infected patients start ART as soon as possible within eight weeks of initiating anti-TB treatment, but at the time lacked any evidence-based research.
Upon enrollment in the CAMELIA trial, all participants started standard treatment for TB, followed either two weeks or two months later by ART. Patients, all of whom had very weak immune systems, were seen at one of five study sites across Cambodia and followed for as long as four and a half years. By the time enrollment closed, 661 patients had been recruited into the study.
At the end of the study, the survival rate in the early ART group was 33 percent higher than that in the late ART group.
The study was also remarkable for its successful level of follow-up. Of the trial’s 661 participants, only 12 were lost to follow-up over the study period, and participants only missed less than one percent of the study’s 8,955 scheduled visits.
“Tuberculosis claims the lives of more than half a million people with HIV worldwide every year,” said Goldfeld, co-founder of the Cambodian Health Committee. “This is a tragedy, because TB is completely curable when diagnosed and treated properly even in a patient with advanced HIV, especially if the patient also receives anti-retroviral therapy.”
Asian Scientist
October 27, 2011
A clinical trial in Cambodia has shown that starting antiretroviral treatment for HIV at two weeks, instead of two months after tuberculosis treatment, increases survival rate by 33 percent in HIV-TB co-infected patients.
Asian Scientist (Oct. 27, 2011) – Timing is everything when treating patients with both HIV and tuberculosis, as demonstrated by researchers at Children’s Hospital Boston and the Immune Disease Institute (IDI) via a large-scale clinical trial in Cambodia.
The study results show that immunosuppressed HIV-TB co-infected patients should be started on ART rapidly at two weeks, rather than two months as current practice, after beginning TB therapy to increase survival rate by 33 percent.
These results were published in the October 20 issue of the New England Journal of Medicine by Prof. Anne Goldfeld of the IDI and Children’s Hospital Boston, and the CAMELIA (Cambodian Early versus Late Introduction of Antiretrovirals) study team.
A collaboration of Cambodian, French, and American physicians and researchers, the CAMELIA trial set out to settle a long-standing debate in the medical community over the relative timing of ART and anti-TB treatment regimens in co-infected patients.
Some have advocated for delaying ART for upwards of two months after initiating anti-TB treatment. They argue that the toxicity of and difficulties in adhering to the two regimens (which together require patients to take seven pills every day), as well as the risk of severe inflammation as the immune system rebounds from HIV’s suppressive influence, create undue burden on patients.
Conversely, those supporting early initiation of ART note that rapid restoration of immune function bolsters the effects of anti-TB treatment.
Latest World Health Organization (WHO) guidelines recommended that co-infected patients start ART as soon as possible within eight weeks of initiating anti-TB treatment, but at the time lacked any evidence-based research.
Upon enrollment in the CAMELIA trial, all participants started standard treatment for TB, followed either two weeks or two months later by ART. Patients, all of whom had very weak immune systems, were seen at one of five study sites across Cambodia and followed for as long as four and a half years. By the time enrollment closed, 661 patients had been recruited into the study.
At the end of the study, the survival rate in the early ART group was 33 percent higher than that in the late ART group.
The study was also remarkable for its successful level of follow-up. Of the trial’s 661 participants, only 12 were lost to follow-up over the study period, and participants only missed less than one percent of the study’s 8,955 scheduled visits.
“Tuberculosis claims the lives of more than half a million people with HIV worldwide every year,” said Goldfeld, co-founder of the Cambodian Health Committee. “This is a tragedy, because TB is completely curable when diagnosed and treated properly even in a patient with advanced HIV, especially if the patient also receives anti-retroviral therapy.”

No comments:
Post a Comment